Learning Healthcare Systems
Learning healthcare systems are systems in which knowledge generation processes are embedded in daily practice to produce continual improvements in care.
What is a Learning Healthcare System?
It is defined by the Institute of Medicine (IoM) as a system in which “science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the delivery process and new knowledge captured as an integral by-product of the delivery experience.”
Professor Friedman, Chair of the Department of Learning Health Sciences at the University of Michigan Medical School, describes a cycle with processes that are common to all Learning Health Systems: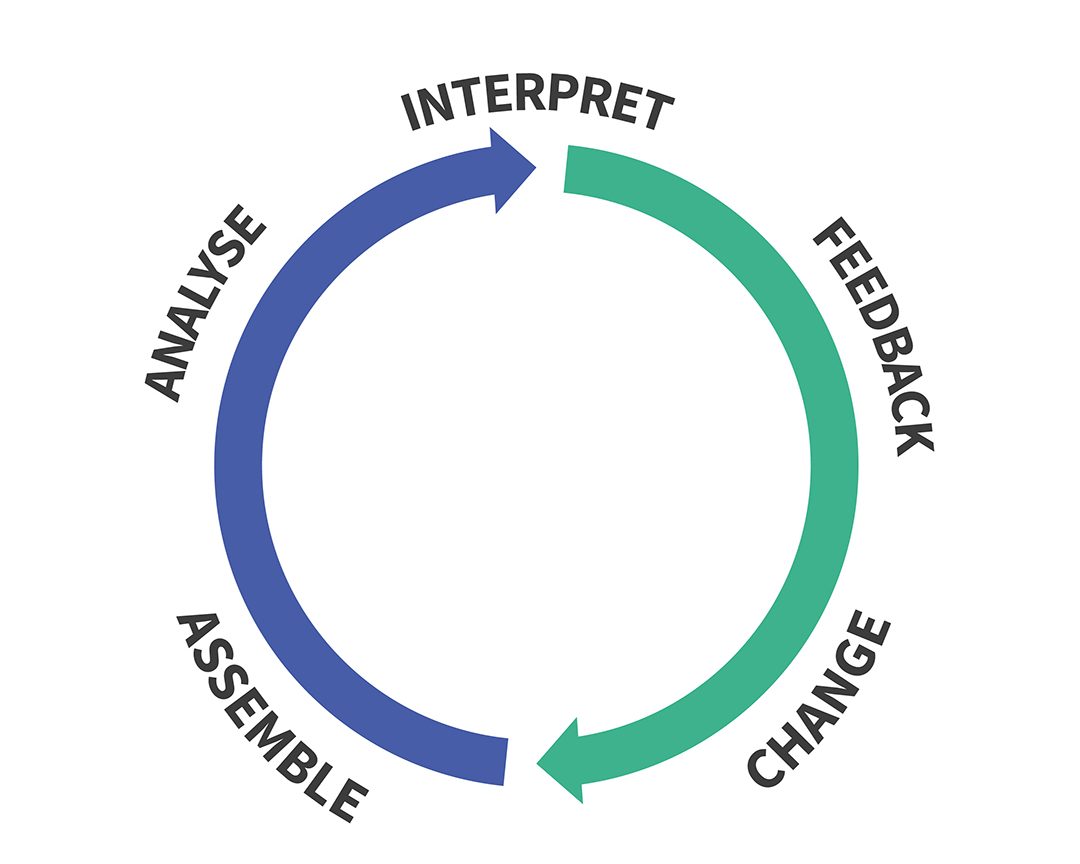
Figure 1: Reproduced from Toward Complete & Sustainable Learning Systems, 2014: https://medicine.umich.edu/sites/default/files/2014_12_08-Friedman-IOM%20LHS.pdf
According to Professor Friedman, any Learning Healthcare System has three components:
- Afferent (Blue) side:
- Assemble the data from various sources
- Analyse the data by various means
- Interpret the findings
- Efferent (Red) side:
- Feeding findings back into the system in various formats
- Changing practice
- Scale: Can be institutional, national, international
According to Paul Wallace, a Learning Healthcare System is a sociotechnical system. The blue/afferent side is made possible by recent technical innovations, but red/efferent side is an enormous interdisciplinary challenge incorporating behavioural psychology, communication science, implementation science, behavioural economics, policy science and organisational theory (Friedman, 2015).
Such systems can be based on any of the cyclical improvement approaches, such as Plan, Do, Study, Act, but they explicitly use technical and social approaches to learn and improve with every patient who is treated. We focus on behaviour change techniques as an effective mechanism to ensure that knowledge generated by Learning Healthcare Systems is fed back into the system to achieve change (the red side of the cycle).
Electronic Health Records provide a data source and a user interface to many Learning Healthcare Systems, but on their own, they do not represent the entire sociotechnical cycle outlined in Figure 1.
There is no single Learning Healthcare System; there are many manifestations, at different scales. It could be a department that tracks its patients’ outcomes in order to learn and improve its practice. It could be a provider that builds predictive models, from elements of its Electronic Health Records, which allow it to forecast demand and reallocate resources more effectively. It could be a national distributed network drawing millions of patient records from multiple providers, to assess the effectiveness of a particular treatment.
Why do we need Learning Healthcare Systems?
Modern medicine has brought significant advances in understanding human health, preventing and managing illnesses, and improving quality of life for patients. In large areas of medicine however, the complexity of the health condition and the heterogeneity of patient characteristics mean that experimental studies such as randomised controlled trials are too costly to conduct. When they are conducted, the exclusion criteria often make it difficult to generalise the results to real patients (Loder, Bunt et al. 2013).
Furthermore, the proliferation of new studies means that it is impossible for practitioners to keep abreast of the latest developments in all but the very narrowest of fields (Davidoff, Haynes et al. 1995). Even evidence-based medicine approaches, such as the development of systematic review methodologies (Sackett, Rosenberg et al. 1996) can only partially address this problem because of the volume and complexity of studies. The net result is that medical practice still relies on gut feeling and all of the associated biases (Matzen 2003, Loder 2015)
In addition to the rapid expansion in the evidence base, health and care faces other challenges from growing and ageing populations, rising levels of chronic illness, constrained budgets, health inequalities, and the proliferation of high cost interventions that bring diminishing returns in terms of the health improvements that they provide. Improvements in productivity are urgently sought. Variations in practice, that cannot be justified, are increasingly seen as unacceptable, but healthcare organisations and clinicians often do not have the capability, opportunity or motivation to drive change, because of other pressures.
A Health Foundation report identified seven key success factors for promoting change at any level in the healthcare system (Allcock, Dormon et al. 2015). The report maps these factors onto eight other models of change dating back almost three decades. Many models of change have been developed and yet successful change remains an elusive goal, suggesting that at least one fundamentally new development will be required to improve the situation.
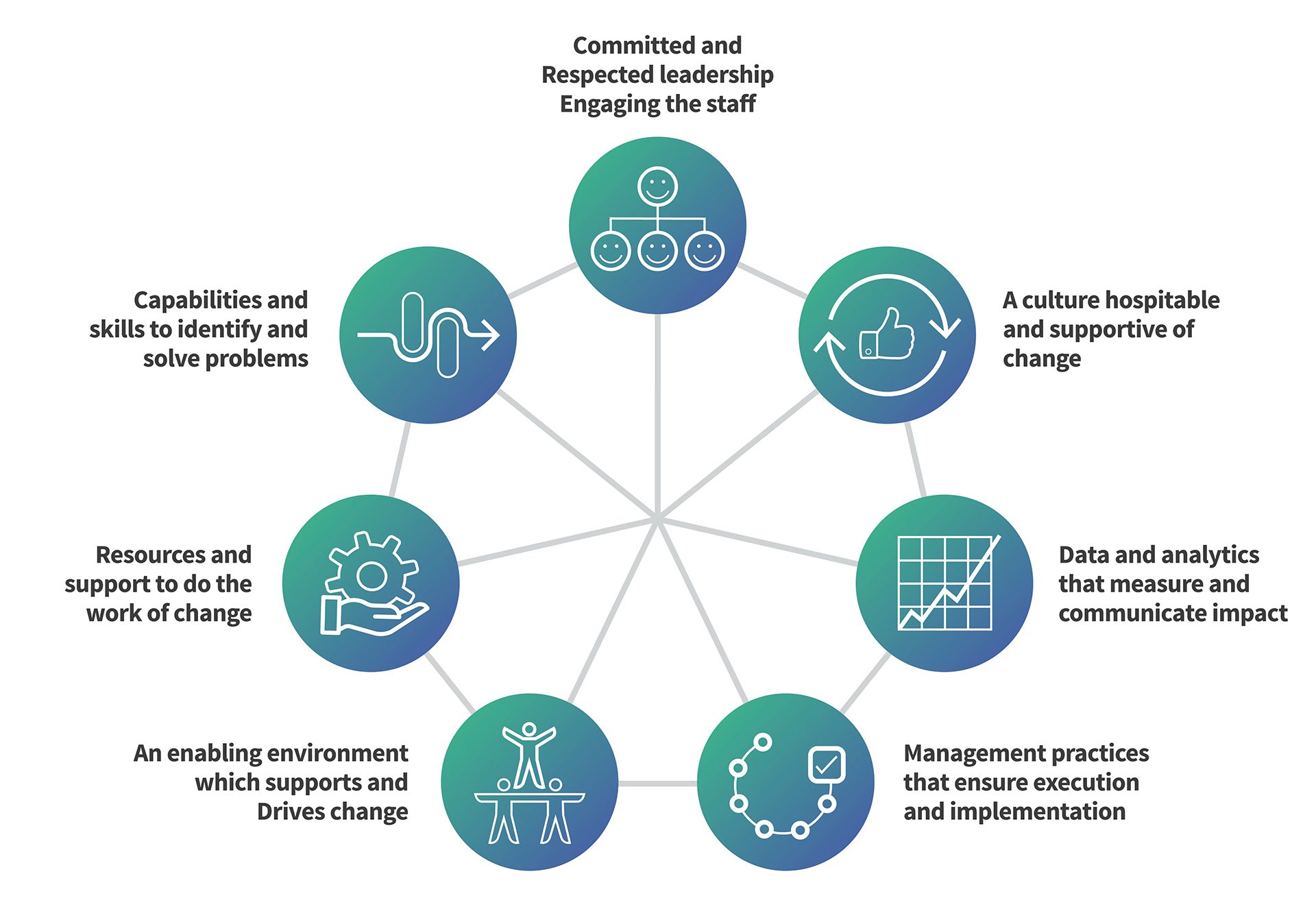
Figure 1: Seven success factors for change in the NHS (Reproduced from Allcock, Dormon et al. 2015)
There are at least three fundamental developments within sight and their realisation could enable Learning Healthcare Systems to facilitate more successful change within healthcare. These developments are:
- Routine data collection and analytics
- Outcomes measurement
- Systematic behaviour change theory and techniques
Routinely collected data has long been used to improve healthcare. The factor that can now help to bring these developments to fruition within healthcare is the development of digital infrastructure. This can automate processes that were previously infeasible, apply enormous computational power and instantly link data recorded in distant geographies. To date, healthcare has been behind other industries in its use of data but the roll out of Electronic Health Records and recent development of standards suggest that this could change.
