Catalyst Project: AI-driven clinical decision-making tool to manage cystic fibrosis
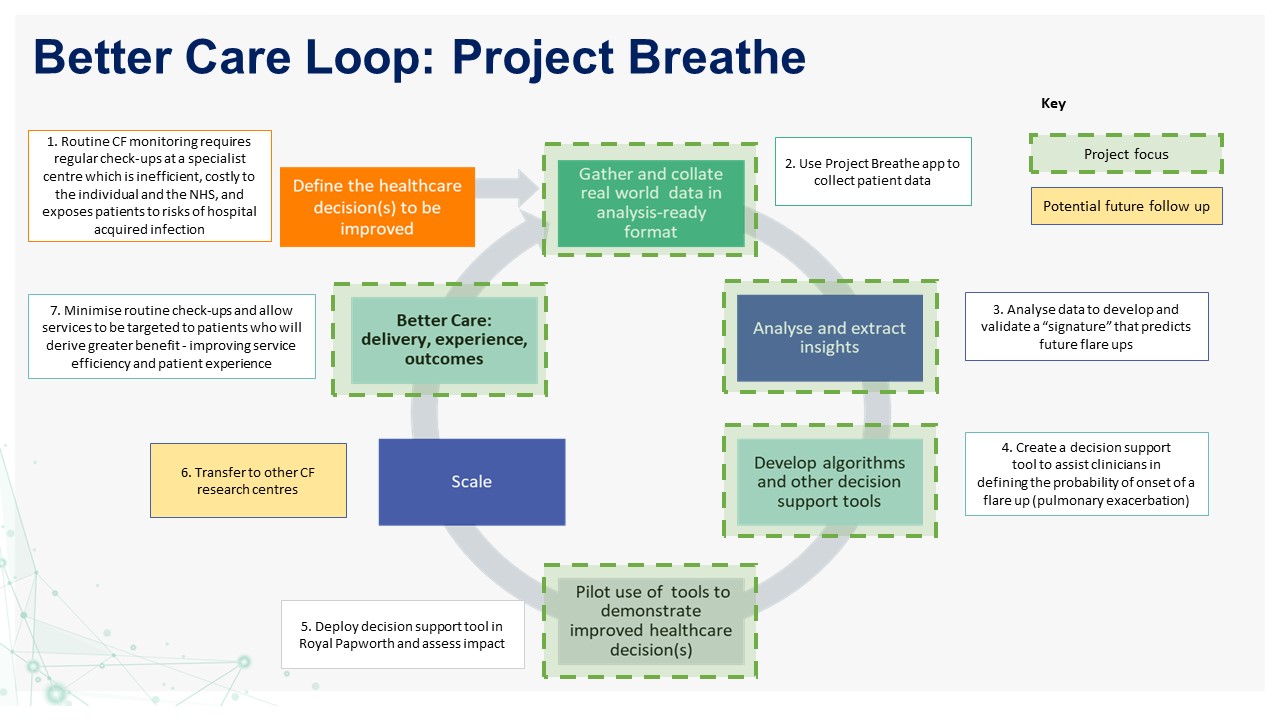
This project, led by Royal Papworth NHS Foundation Trust, aims to use AI-machine learning to understand why pulmonary exacerbations happen in people with cystic fibrosis (CF). They plan to develop a tool to assist clinicians in deciding when to treat the patient, and therefore reduce routine outpatient visits

The challenge
Management of chronic conditions results in a huge burden of care on healthcare delivery systems. CF, a genetic disorder diagnosed at birth, is a lifelong condition resulting in premature death caused by flare-ups in the lungs with repeated rounds of infection, inflammation and scarring. These flare-ups (pulmonary exacerbations) are hard to identify in their early stages so treatment is often delayed. Current management requires a routine check-up at a specialist centre every 6-8 weeks, which is costly to the individual and the NHS, and exposes patients to additional risks of cross infection in hospital.
The solution
The Cystic Fibrosis Trust has been exploring potential ways to reduce the burden of care by using blue-toothed devices for home monitoring. Their study, SmartCareCF, demonstrated the feasibility of daily measurements, and these insights have guided the design for this Catalyst project led by Royal Papworth NHS Foundation Trust.
Artificial intelligence analysis of the SmartCareCF data has enabled the development of an algorithm that predicts a future flare-up by about 11 days. The team aim to build on the success and learnings from the SmartCareCF study by collecting real-world data to test the “signature” in real-time. This analysis will validate the tool and provide an approach to recognise and treat CF flareups earlier. The same real-world data can be used to ensure more efficient use of hospital centre outpatients by abolishing routine check-ups and seeing people when they most need professional healthcare.
The impact and outcomes
Earlier identification of a potential flare-up and appropriate treatment may reduce adverse consequences for patients such as lung scarring, hospitalisation and two weeks of antibiotics dosed directly into the bloodstream. In addition, safely reducing routine outpatient visits will significantly lower the burden of care for people with CF and their families. The ultimate goal is to change clinical practice, by tailoring the clinic visit around the patient rather than the patient around the hospital clinic. By using home-monitoring, visits will be defined by need of the individual, seeing the appropriate healthcare specialist at the right time.
Project Team
Project Director: Charles Haworth, Royal Papworth NHS Foundation Trust
Team members: Andres Floto, University of Cambridge
John Winn, Microsoft Research, Cambridge
Collaborators:
Charity: Dr Janet Allen, Cystic Fibrosis Trust, London
Industry: Kirsty Hill, Magic Bullet



