Development of a learning system to optimise anticholinergic medication prescribing for older people living with frailty
Overview
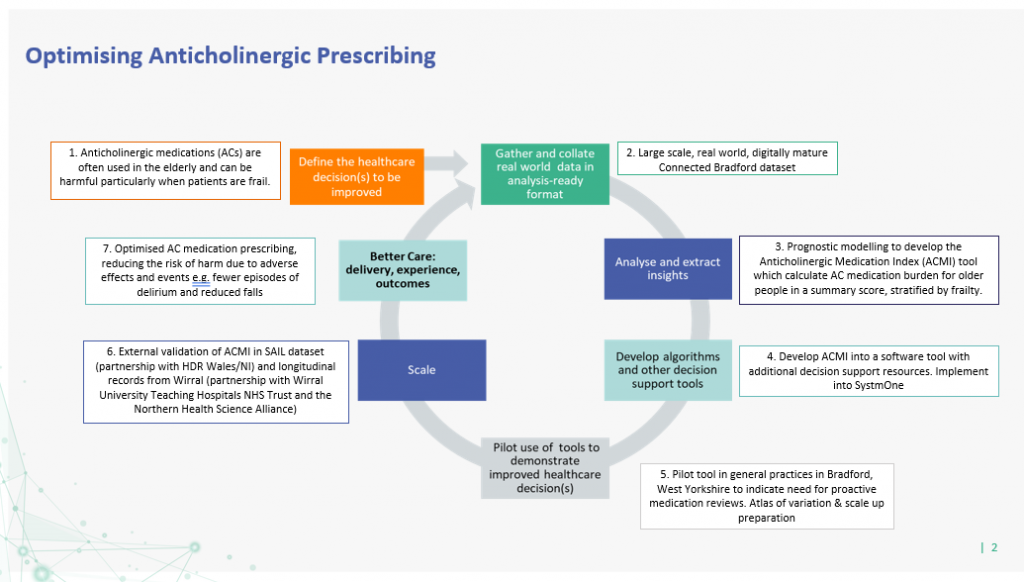
This project aims to develop a tool to help doctors and pharmacists review a patient’s broader medical history to allow more appropriate prescribing of anticholinergic medications. This will help older people living with frailty by reducing the risk of harmful side effects caused by these medications, which can lead to hospital admissions.
The Challenge
The NHS needs to improve support for GPs to optimise the medications prescribed to frail older people to avoid harmful effects. This project focuses on anticholinergic medications (ACs) used to treat bladder, bowel and mood problems. Common side effects of these medications in older people include confusion and falls that often lead to hospital admission.
Around 20% of older people are prescribed AC medications and those living with frailty are recognised as being particularly sensitive to the adverse effects of AC medications. These patients are also more likely to suffer from multiple long-term conditions. The combination of medications used to treat these conditions increases the risk of additive effects leading to harmful AC drug-drug interactions.
A range of tools have been developed to calculate AC medication burden to help guide practitioners in prescribing for older people. However, these tools have not been optimised in terms of predicting adverse outcomes, and none have been made easily available across UK clinical information systems in ways that could underpin a ‘learning system’.
The Solution
This project will develop the Anticholinergic Medication Index (ACMI) tool to calculate AC medication burden for older people in a summary score, stratified by frailty. The tool will be developed using prognostic modelling techniques and tested using anonymised routine data from the Connected Bradford dataset of over 180,000 people aged 65 years and older to see how well the score predicts being admitted to hospital with confusion or a fall.
This score will run in a computer-based system designed with pharmacists and doctors to help them review patients’ medicines and reduce harm from ACs.
The ACMI will be developed into a software tool with additional decision support resources and piloted in general practices in Bradford, before being offered for broader national use.
The Impact and Outcomes
The overall aim is to improve quality of life and clinical outcomes, and save NHS and social care costs. This project will benefit older people living with frailty by optimising AC medication prescribing, reducing the risk of harm due to adverse effects and events. It is anticipated that care will improve as a direct result as individuals will experience fewer episodes of delirium and reduced falls. Improvement in these outcomes will have considerable benefits for the NHS and social care services, with associated wider societal and economic benefits.
Better Care Loop
Project Team
Andy Clegg, Professor of Geriatric Medicine, University of Leeds and Bradford Royal Infirmary
Sarah Rodgers, Professor of Health Informatics, University of Liverpool