Antithrombotic use shown to improve COVID-19 outcomes in a nationwide atrial fibrillation cohort
11 March 2022
Research from the BHF Data Science Centre’s CVD-COVID-UK Consortium suggests use of blood-thinning medications in patients with cardiovascular disease is associated with lower risk of death from COVID-19.

New research published today from the BHF Data Science Centre’s CVD-COVID-UK Consortium suggests use of blood-thinning medications in patients with cardiovascular disease is associated with lower risk of death from COVID-19.
The study looks at patients with atrial fibrillation, who have abnormal heart rhythm and a higher risk of stroke. In these patients, blood thinning medications called antithrombotics are recommended to reduce stroke risk. Recent evidence also suggests that people already taking this kind of medication have improved outcomes from COVID-19.
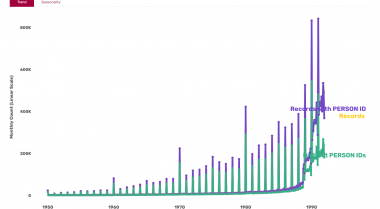
Using data from almost 1 million atrial fibrillation patients, the researchers confirmed pre-existing use of blood thinning medication was associated with a lower risk of death, but a higher risk of hospitalisation from COVID-19.
Alex Handy, lead researcher of the study, said “We observed that people already taking antithrombotics were marginally less likely to die from COVID-19, but were also marginally more likely to be hospitalised. We saw the same pattern in people taking other blood thinning drugs called anticoagulants.
“This pattern could be a result of people taking this kind of medication being more likely to access healthcare, but it may also mean that antithrombotics only help in the most serious cases of COVID-19.
“Although the observation of an association between antithrombotics and lower odds of COVID-19 death does not mean we can conclusively say that taking these drugs directly lower the risk of COVID-19 death, the findings in this study provide a further incentive to ensure that people with atrial fibrillation, and who are already eligible for antithrombotics, are prescribed and take them.”
Previous evidence suggests as many as one third of patients with atrial fibrillation who are at high risk of stroke are not on the best kind of blood thinning medication, or are taking no medication at all, making research like this important to further incentivise the use of these drugs for patients who need them.
The study is the largest scale evaluation of blood-thinning medications to date, using datasets covering GPs, hospitals, pharmacy dispensing, death registrations and COVID-19 testing and vaccination for 56 million people in England.
It was supported by the BHF Data Science Centre, which is a partnership between Health Data Research UK and the British Heart Foundation. The centre works closely with patients, the public, NHS organisations, researchers, and clinicians to promote the safe and ethical use of large-scale data for research into the causes, prevention and treatment of all diseases of the heart and circulation.
The research was conducted by members of the CVD-COVID-UK consortium, a National Institute for Health Research (NIHR) and British Heart Foundation (BHF) flagship project led by the BHF Data Science Centre at Health Data Research UK. The CVD-COVID-UK consortium is a collaborative group of more than 260 members from over 50 institutions across the UK, working together with patient and public contributors to understand the relationship between COVID-19 and cardiovascular diseases such as heart attack and stroke in the UK population.
Cathie Sudlow, Director of the BHF Data Science Centre, said “This research is the perfect example of the large-scale, data-driven approaches the BHF Data Science Centre is enabling to improve cardiovascular health in the UK and beyond.
“By harnessing the power of NHS Digital’s resource of over 56 million people’s health data, via the CVD-COVID-UK consortium, research like this represents a step change in the UK’s capability as a world-leading environment for cardiovascular research and innovation.
“The BHF Data Science Centre is thrilled to have been able to contribute to these important results that will help inform the use of blood clotting medicines to improve the public’s cardiovascular health and provide better outcomes for millions across the UK.”
Edit: This paper was selected by our Impact Committee in May as their Open Access Publication of the Month.
The committee said: “We scored the paper high on team science and scale as it brings together several researchers from across the four nations and uses data derived from a cohort all individuals registered with a GP in England. The project also included some patient and public involvement in reviewing and approving the project.
“This paper provides important information regarding both antithrombotic use in patients with atrial fibrillation high risk for stroke and the potential for these medications to reduce mortality in these patients if they develop COVID-19.”