Computable knowledge Part 1 of 2: What is it and why do we need it to build a Learning Health System?
19 February 2021 | Author: Philip Scott, Researcher
HDRUK is all about health data, right? Wrong! Data on its own is meaningless and useless. Data collection only becomes worthwhile when we derive actionable insight from it – a piece of knowledge.
Biomedical research knowledge has traditionally gone into academic journals, where typically it will sit for 15 years or so until someone does a systematic review and (perhaps) it eventually gets into a NICE guideline and over a few more years (perhaps) begins to change clinical practice.
That kind of knowledge, even when it gets into the practice guideline, is usually narrative knowledge. (See diagram below – with permission, amended from original by Andy Mitchell, NICE.
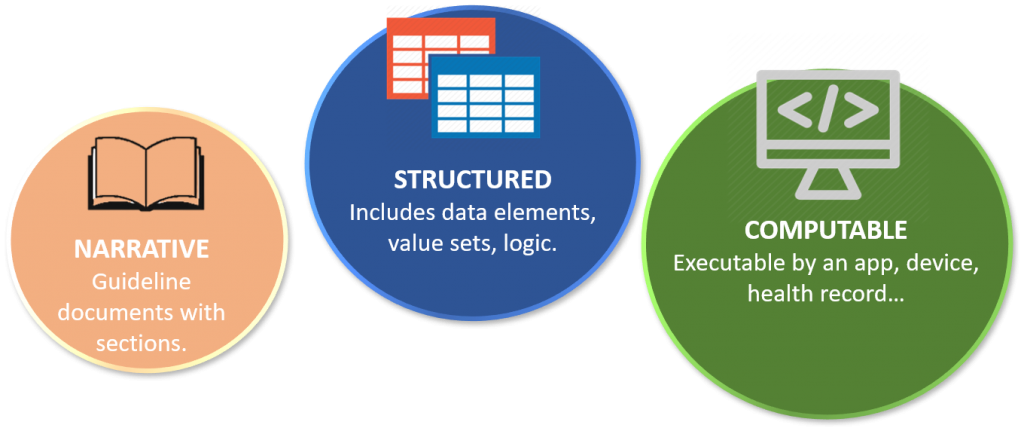
The guideline may turn it into structured knowledge and possibly even explicit knowledge – for example, a cardiac risk score or specified diagnostic investigations. Guideline committees generally don’t go any further than that, but knowledge can – it can become computable!
Can computable knowledge help routine practice? Clinical decision support tools are not perfect, but have been shown to be effective in improving practice when well designed and implemented. There are many kinds of decision support in regular use, such as prescribing guidance, early warning scores, and medical device alerts. Decisions remain with the responsible clinician, but computable knowledge makes sure they have the best guidance in the easiest form to act upon.
Right now, each decision support tool has to separately hand-craft the guidelines into software – creating obvious “translation” risks many times over. Every time there is a guideline revision, there is a huge cascade of repeated, independent, manual software updates. What we really need is a library of computable knowledge in formats that meet international standards that can be published once, updated once, shared automatically and implemented in all the subscribing decision support apps, devices and systems (subject of course to appropriate validation, governance and curation).
As shown in the diagram below – courtesy of Prof Charles Friedman, University of Michigan – computable knowledge is a keystone in the Learning Health System. Knowledge produced in the Data to Knowledge (D2K) phase is no longer “lost” in the literature, but rapidly deployed into operational health and care systems in the Knowledge to Performance (K2P) phase and its impact assessed in the Performance to Data (P2D) phase – see: umich.edu.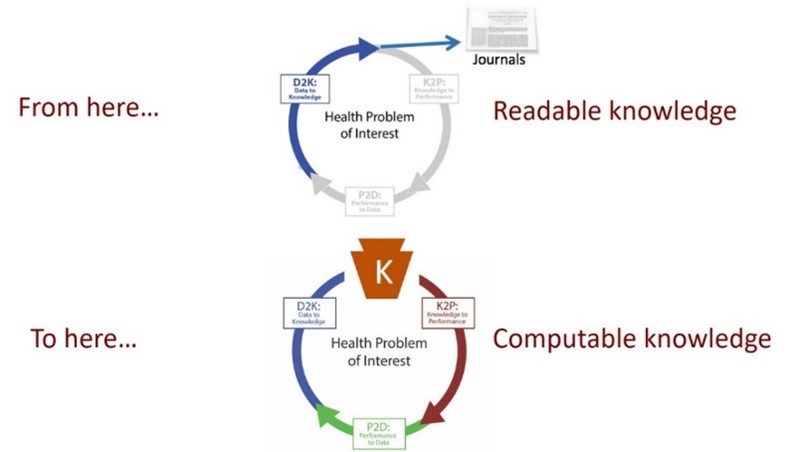
How can HDR UK contribute to this? Part two of this blog series – published Friday 26 February – will explain further.